Master Social Anxiety with Cognitive Behavioral Therapy: A Helpful Guide
This article includes recommendations for an online therapy service and a workbook that helps with social anxiety. By using our links, it’s possible that you receive a discount, and we may earn a commission, which supports the maintenance of our website.
Social anxiety disorder encompasses more than just challenging emotions like fear, shame, and sadness; it also involves profoundly negative thoughts and detrimental behavioral cycles.
Numerous experts assert that the foundation of social phobia doesn’t solely rest on these pessimistic cognitions but also on the potent inclination to evade anxiety-inducing social situations, which frequently serves as the genesis of its development.

Cognitive Behavioral Therapy (CBT), when applied to social anxiety, directly confronts these counterproductive patterns, striving to transform them, thereby fostering substantial alleviation of social fear and discomfort.
Currently, CBT stands tall as the preferred and recommended approach for treating social anxiety.
This article delves into the reasons underscoring its preeminence and dissects its fundamental components for a comprehensive understanding.
A. Understanding Social Anxiety Through CBT
The Cognitive Model of Social Anxiety
In comprehending the workings of CBT and its efficacy in alleviating social anxiety, it’s crucial to delve into the cognitive model that underpins the disorder.
While there are several cognitive models, in this article we’ll spotlight the one most widely applied, crafted by psychologists David Clark and Adrian Wells in 1995.
The Catastrophic Cascade
According to this model, a specific social situation triggers a cascade of negative thoughts, frequently spiraling into catastrophic proportions.
This train of thought is often rooted in past traumatic social experiences, serving as a blueprint for anticipation of potential disaster.

For instance, consider Erica, who, a decade after being ridiculed during a school presentation, now faces a similar scenario in front of colleagues.
The memories of her past experience resurface, kindling a barrage of detrimental thoughts.
“I’m terrified they’ll laugh at me again, just like back in school. I must not show any sign of anxiety, or they’ll deem me odd and mock me.“
The Vicious Loop Takes Shape
At this juncture, a vicious cycle sets in motion, where negative thoughts, heightened self-consciousness, anxiety symptoms, and safety behaviors intertwine, bolstering one another.
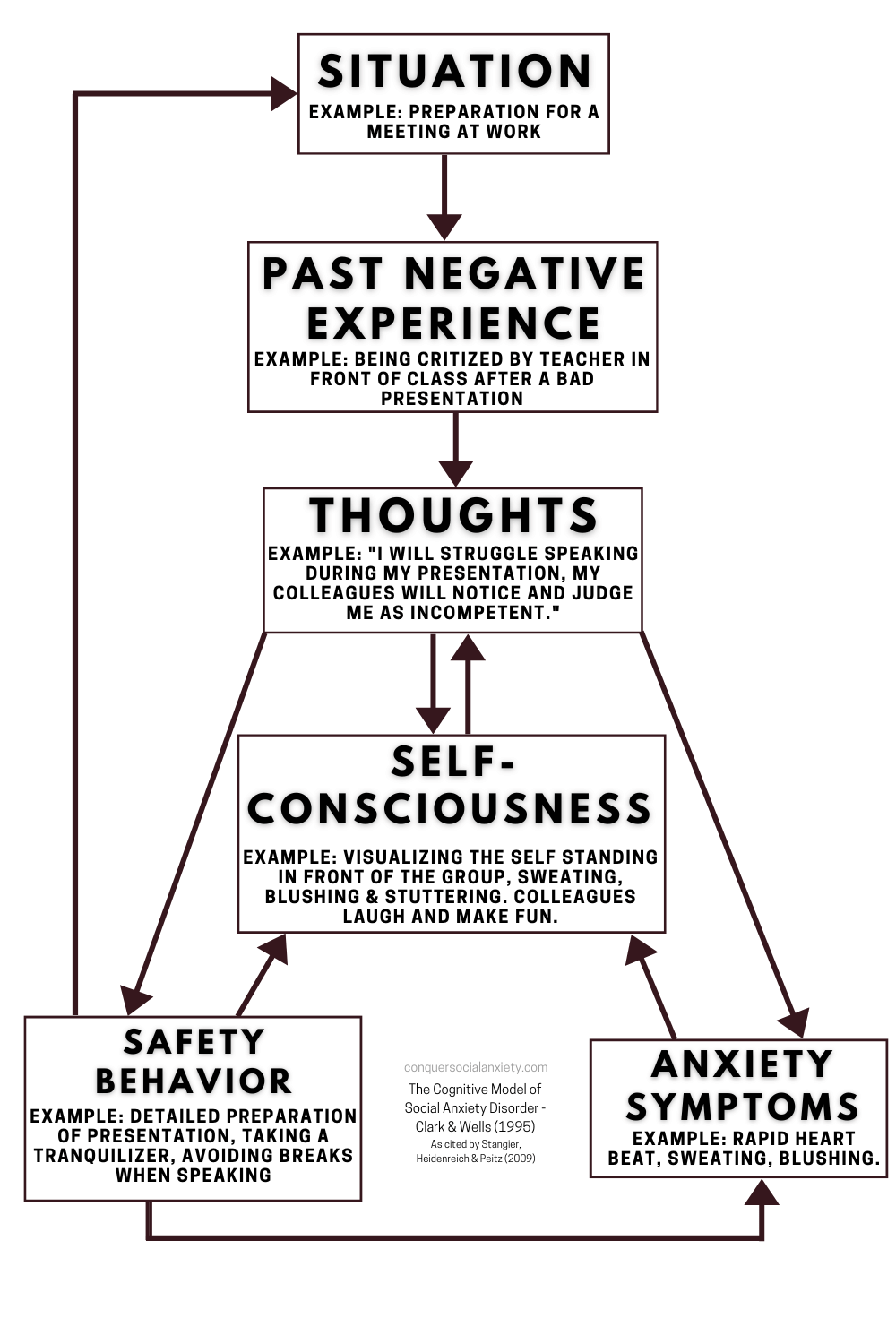
Erica’s heightened self-awareness prompts a surge of anxiety, palpably manifesting as rapid heartbeats and flushed cheeks.
This intensifies her mental preoccupation with how she appears to others, further fueling negativity.
“They can see how nervous I am. My blushing, shaky hands, and cracking voice must be apparent. I must conceal my anxiety.“
In response to these fears, Erica employs so-called “safety behaviors” – strategies to thwart her apprehended worst-case scenarios and safeguard her public image.
She grips her notes tightly to obscure trembling hands, speaks softly to cloak voice cracks, and attempts to suppress anxiety and its accompanying physical sensations.

Safety Behaviors Backfire
Ironically, while Erica believes these tactics shield her from anticipated outcomes, they heighten self-consciousness and amplify feelings of insecurity.
Her preoccupation with self takes precedence over her presentation task, ultimately eroding her performance.
Furthermore, her fixation on negative outcomes obscures positive social cues, such as approving nods from colleagues, which could ease her anxiety.
Attempting to stifle her anxiety-related manifestations paradoxically reinforces them. Stress and anxiety intensify, deepening the psychological conundrum she finds herself in.
Take a look at the graphic below, where the red arrow vividly demonstrates how safety behaviors can inadvertently tighten the grip of the social anxiety loop.
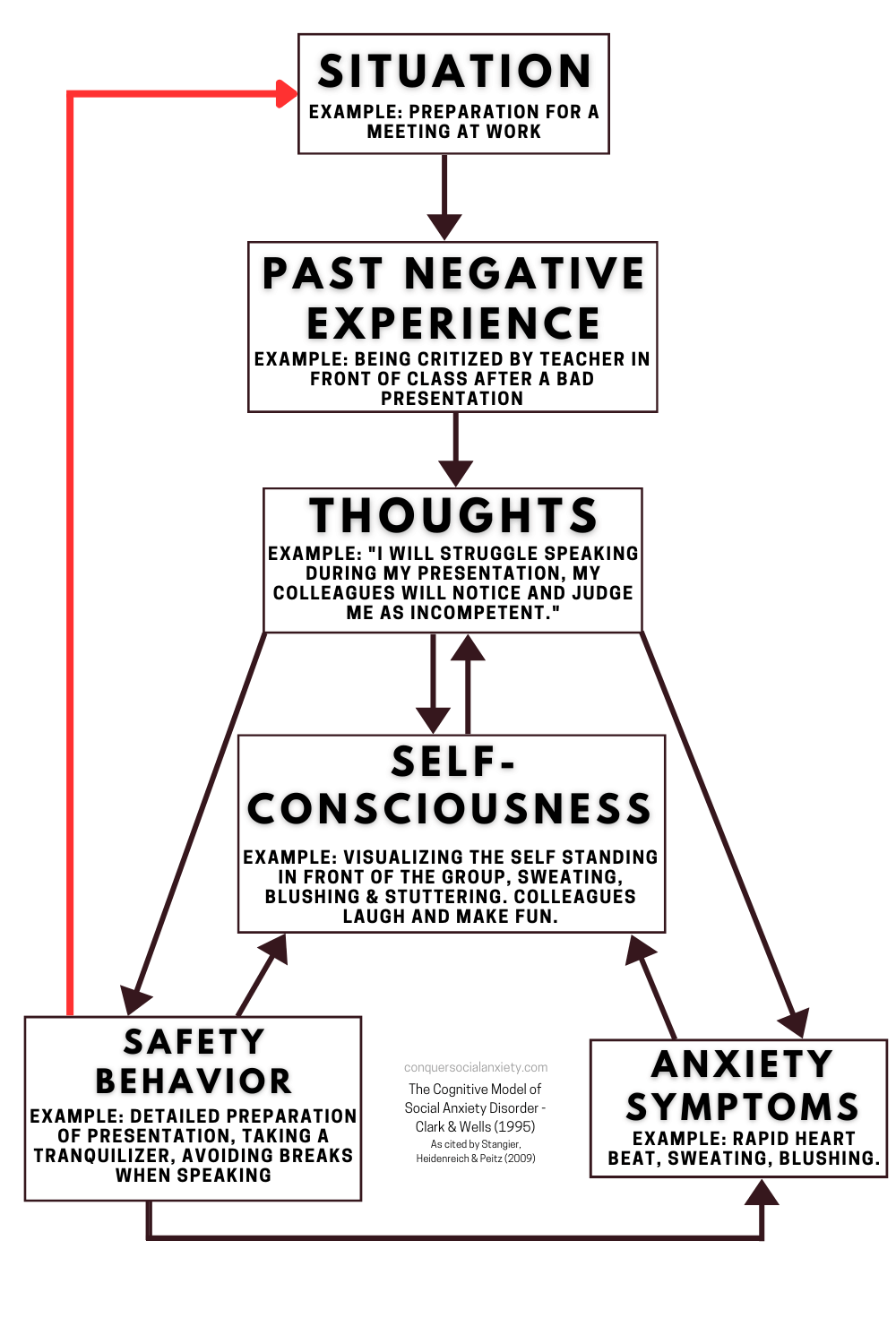
When situations are approached with cautious attempts to mitigate potential negative outcomes, these behaviors prevent genuine engagement with the source of fear.
Consequently, the fear response persists, as the opportunity for corrective experiences remains elusive.
Breaking Down the Feedback Loop
The graphic above illustrates a critical loop from safety behaviors back to the origin of negative thoughts, revealing the role of safety behaviors and avoidance in perpetuating social anxiety.
CBT treatment zeroes in on this cycle to effect change.

Remarkably, Erica’s decision not to avoid the presentation is a positive stride, though her safety behaviors impede transformative experiences that could alleviate future anxiety.
Strangely, safety behaviors often yield the very results they aim to avert, as seen in Erica’s firm grasp on notes exacerbating her tremors or her attempts to minimize cracks in her voice by speaking with low volume actually heightening perceptions of insecurity
A Cycle of Amplified Anxiety
Erica’s story underscores how safety behaviors and post-event processing, where she replays events negatively in her mind, exacerbate anticipatory anxiety about future social situations.
This self-reinforcing cycle maintains and intensifies the social anxiety disorder.
Halting the Cycle with CBT
Now, let’s explore how CBT intervenes to halt this cycle, liberating individuals from the grip of maladaptive thought and behavior patterns.
B. How Does CBT Help With Social Anxiety?
CBT helps with social anxiety by changing the way people think and behave. It encourages to question and readjust negative beliefs, to focus on outward stimuli instead of internal sensations, to seek repeated exposure to the feared situations, and it teaches social skills when there is a deficit.

Targeting Modifiable Components
Within the web of the cognitive model of social anxiety, certain components stand as modifiable, while others remain immutable.
The trauma of past social experiences or the direct control over anxiety symptoms are examples of aspects beyond immediate alteration.
Nonetheless, there are components within our grasp for transformation, precisely where CBT comes into play.
By addressing these malleable components, CBT effectively mitigates anxiety symptoms. We’ve visualized this concept in the graphic below.
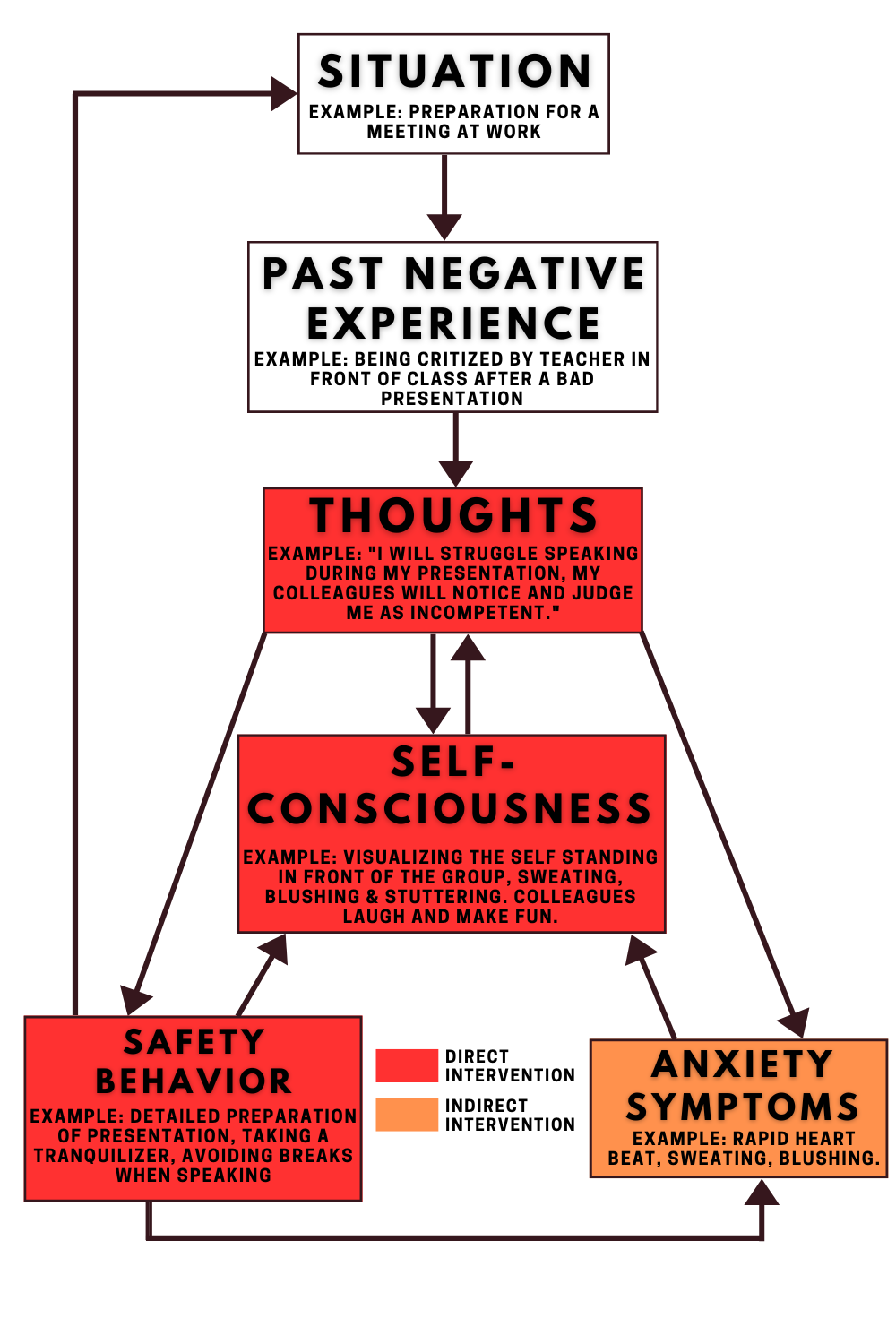
The elements emphasized in red signify the core of CBT’s focus, directly affecting these aspects to instigate positive transformations in anxiety symptoms. Meanwhile, the anxiety symptoms highlighted in orange are addressed indirectly through this approach.
Transforming Thought and Behavior
The bedrock of CBT’s efficacy in combating social anxiety lies in its dual approach – reshaping thought processes and recalibrating behavioral responses.
CBT prompts individuals to scrutinize and recalibrate negative beliefs, shift focus from internal sensations to external cues, embrace repeated exposure to feared scenarios, and even fortify social skills if deficits exist.

Charting the Cognitive Course
Cognitive restructuring emerges as a pivotal element within CBT. This aspect homes in on unraveling unproductive thoughts and beliefs that are particularly burdensome for those grappling with social anxiety.
Take Erica once more: if she clings to beliefs of being unlikable and insignificant, she not only grapples with plummeting self-esteem but also navigates acute anxiety during potential scrutiny.
Within CBT, these deeply rooted negative core beliefs burgeon into intermediate beliefs – akin to rigid guidelines and attitudes about the self, others, and the world.

For instance, Erica’s intermediate beliefs might encompass:
- “If others detect my insecurity, they’ll disdain me.“
- “I must retain emotional control to evade rejection.“
- “Confidence is the sole gateway to competence.“
- “I’m ill-equipped to cope with rejection or pity.“
In real-life scenarios, these intermediate beliefs spark automatic negative thoughts – anxiety-laden notions unique to each situation.
- “I’m jittery; I’ll make a spectacle of myself.“
- “Laughter – they’re mocking me.“
- “Trembling – must calm down swiftly.“
A three-tiered structure illustrates this progression: core beliefs shape intermediate beliefs, which then ignite automatic negative thoughts.
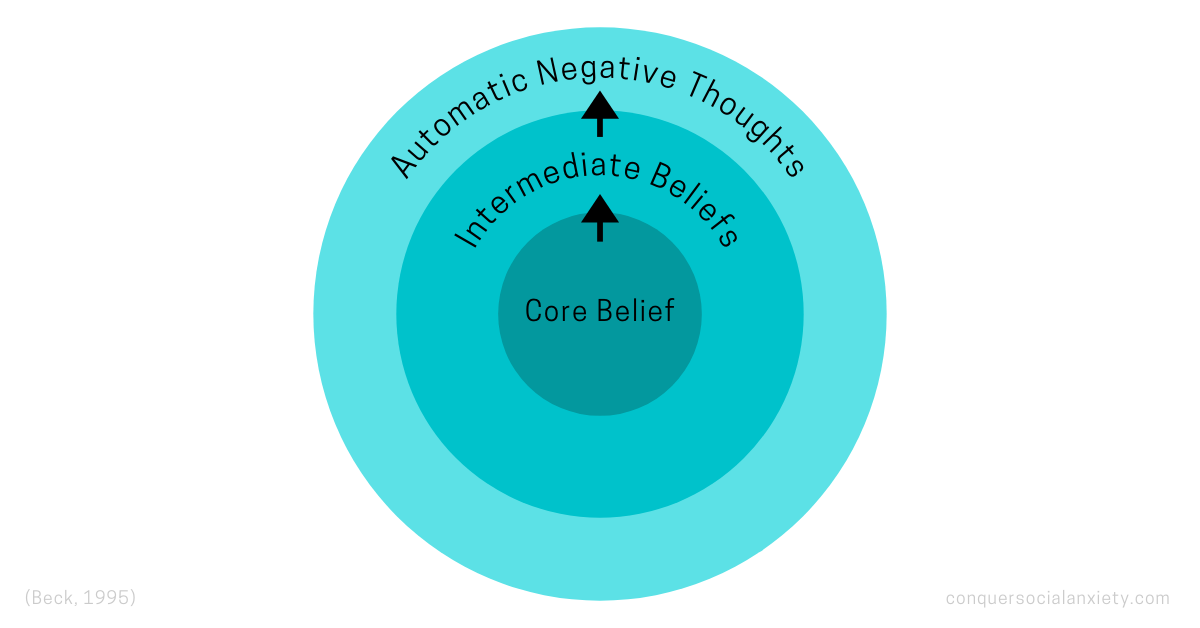
CBT intervenes through cognitive restructuring, a repertoire of techniques for discerning and overhauling maladaptive thought patterns.
By delving into specific automatic negative thoughts, therapist and patient uncover underlying intermediate beliefs, serving as a springboard to deduce core beliefs – fundamental self-assumptions.
Through rigorous scrutiny, patient and therapist evaluate the accuracy and utility of these thoughts and beliefs.
When deemed inaccurate or counterproductive, patients reconstruct their cognitive framework, forging more accurate and constructive thought patterns.

Some techniques encompass:
- Socratic questioning: Provoking rational, logical thinking to interrogate presumed truths.
- Collecting evidence: Seeking and assembling proof for alternative beliefs, facilitating their adoption.
- Identifying rational alternative explanations: Shifting from personalization to diverse explanations for others’ behaviors.
- Decatastrophizing: Diminishing the tendency to magnify trivial issues.
Over time, under the guidance of an adept therapist, cognitive restructuring has been proven to reduce negative social cognitions and amplify positive ones, ultimately diminishing social anxiety (Taylor et al., 1997).

Simultaneously, patients receive education about the pitfalls of fixating on self and internal sensations during social tasks.
This knowledge impels them to pivot their focus outward, honing in on the task itself.
With practice, this shift diminishes self-consciousness in anxiety-inducing scenarios.
Exposure Exercises: Taming the Fear
CBT’s behavioral arm confronts unconstructive behavioral patterns head-on.
In social anxiety’s case, this translates to confronting the inclination to avoid distressing situations and resort to safety behaviors.
The remedy: exposure exercises.

Exposure to the feared social situations is a major element of CBT for social anxiety. When carried out in the right way, it can have profound and often even quick anxiety-reducing effects. To be effective, exposure should be gradual, long enough, and repeated several times.
Vital to CBT, exposure to the feared situations wields transformational potential. Carried out meticulously, it can yield rapid and profound anxiety reduction.
Key to its success are the principles of gradual progression, duration, and repetition.
However, social anxiety, akin to phobias, maintains its grip despite exposure efforts. The culprits are safety behaviors, as already highlighted in the cognitive model (Heimberg, Brozovich, & Rapee, 2014).
Erica’s story underscores this; she lowered her head to mask her blush, inadvertently amplifying her insecurity. Safety behaviors hamper transformative experiences that could alleviate future anxiety.

CBT practitioners emphasize that effective exposure exercises must eschew safety behaviors entirely.
Prior to exposure, patients build an exposure hierarchy – a tiered list of social situations from mildly distressing to extremely challenging.
Take a look at an example of an exposure hierarchy for someone fearing the spotlight:
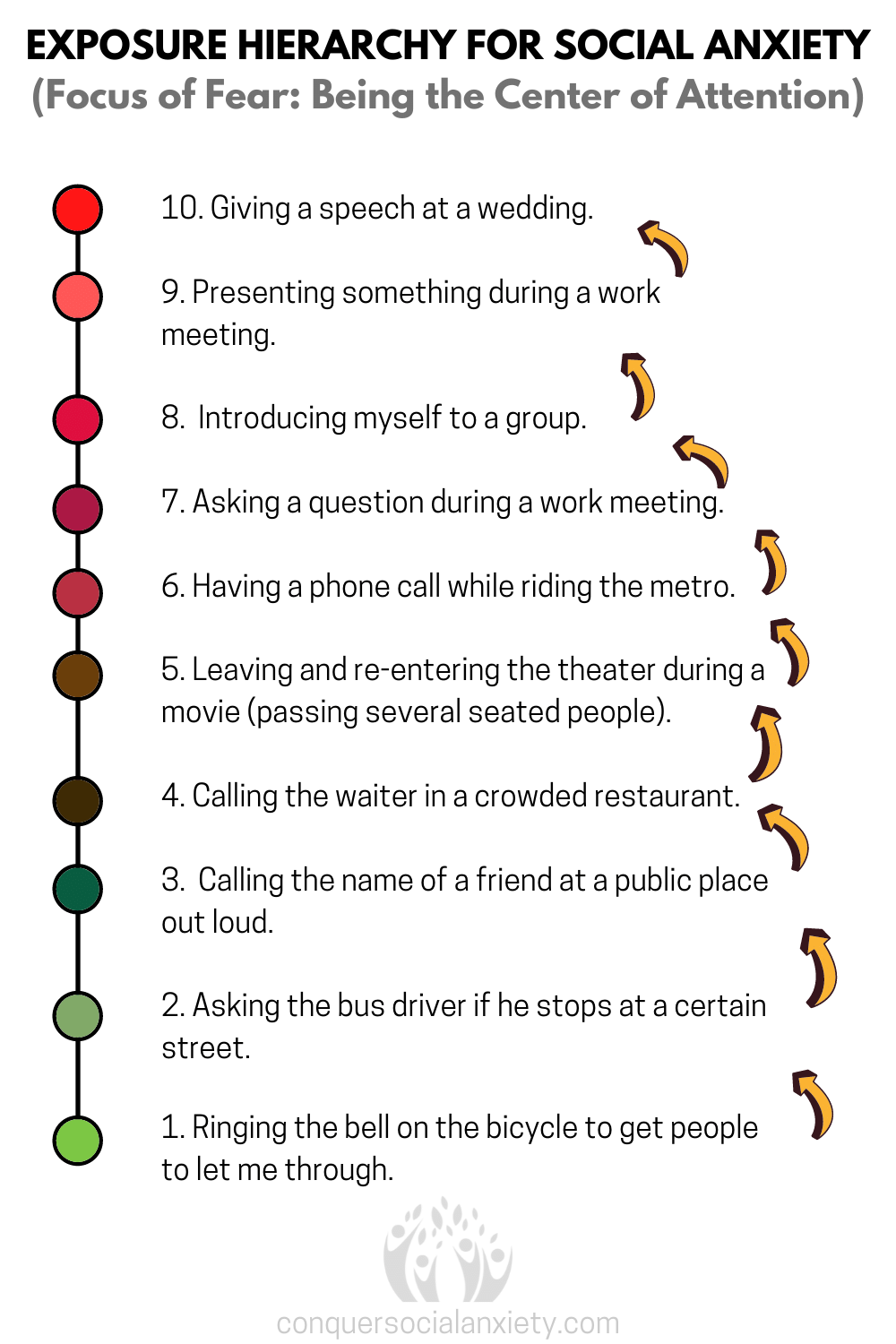
Note the gradual progression, starting with mildly uneasy situations (1-3), advancing to considerably challenging ones (4-7), culminating in scenarios evoking severe anxiety (8-10).
Patients tackle these situations systematically, commencing from the bottom and ascending as anxiety lessens.
In the initial stages, therapists often accompany patients during these exercises.
Gradual, controlled, and repetitive exposure retrains the brain, debunking the perceived danger associated with these situations.
This process, known as habituation and extinction learning, forms the crux of CBT’s behavioral aspect.
Ineffectual safety behaviors, frequently maintaining anxiety despite exposure, are tackled head-on through this exposure-based approach.

Mastering Social Skills
While many grappling with social anxiety possess an awareness of appropriate social behavior, anxiety often inhibits practical implementation.
However, for some, genuine social skills deficiencies exist due to limited opportunities for socialization during childhood.
Enter Social Skills Training (SST), an adjunct to standard CBT.
Standardized CBT for social anxiety disorder does not address specific social skills, as most affected people know how socially appropriate behavior looks like. However, some people have actual deficits in their social abilities, which is then addressed through social skills training (SST).

Patients, guided by therapists, pinpoint problem areas – conversational initiation and conclusion, open and friendly introductions, saying ‘no‘ or declining invitations, asserting oneself, and non-verbal behaviors.
Role-play and therapist-guided correction fine-tune these skills.
Adding SST to CBT proves beneficial (Beidel, Alfano, Kofler, & Rao, 2014), although most social anxiety sufferers don’t require this specialized component.
Generally, social skills deficits remain an exception rather than the norm.
C. How Effective is CBT for Social Anxiety Disorder?
With a comprehensive grasp of how CBT combats social anxiety, it’s time to scrutinize its real-world efficacy. Let’s delve into the realm of empirical evidence to gauge the true impact of CBT.
Examining CBT’s Reach
A systematic review (2015) found that about 45-55% of people with social anxiety disorder (SAD) experience a significant symptom reduction following CBT treatment and a recent meta-analysis (2018) reported that about 40% no longer suffer from SAD after a standardized CBT intervention.
These studies succinctly encapsulate scientific findings, illustrating the significant benefits that many SAD sufferers reap through CBT treatment (Loerinc et al., 2015; Springer, Levy, & Toling, 2018).
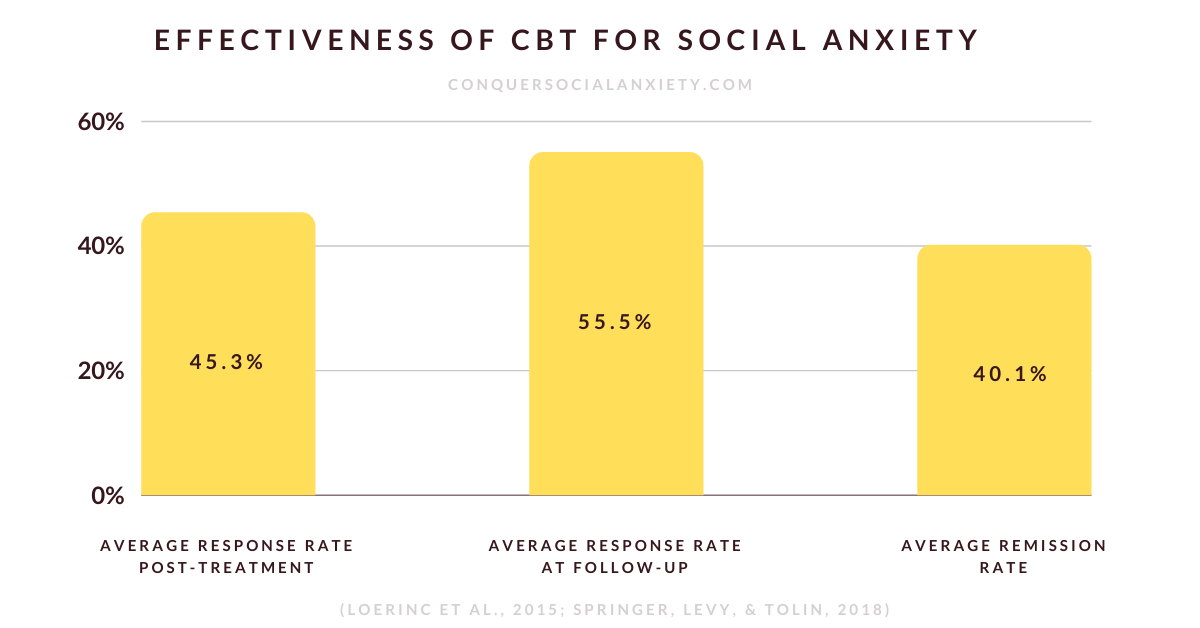
Interpreting the Numbers
While these figures might appear modest on the surface, it’s vital to contextualize them within the broader landscape of psychological treatments for anxiety disorders.
Across the spectrum of psychological interventions, response rates for anxiety disorders typically hover around the 50% mark.
Thus, CBT’s success rates, while seemingly falling within the same range, hold substantial promise given the complex nature of social anxiety.
The complexities of social anxiety necessitate a nuanced approach, rendering each percentage point of progress an accomplishment of immense significance

Exploring Alternative Avenues
For those who may not find the standard CBT approach suitable or effective, a realm of alternative options exists.
We’ve compiled an extensive overview of these alternatives within our comprehensive therapy guide, catering to diverse needs and preferences.
Feel free to click here to access the full article. It not only offers a comprehensive overview of scientifically validated therapies for social anxiety but also equips you with essential insights to initiate your therapy journey confidently.
D. How Long Does CBT Take to Work for Social Anxiety?
Accelerated Relief with CBT
Curious about the temporal trajectory of CBT’s impact on social anxiety? The realm of timeframes reveals a promising prospect.
CBT is renowned for its rapid efficacy, often leading to reduced social anxiety within weeks.
CBT can reduce social anxiety within a matter of weeks, especially when exposure exercises are carried out soon into the treatment process and the patient adheres to the homework assignments. This way, CBT can work right from the moment of treatment initiation.

However, it’s crucial to underscore that treatment outcomes are inherently diverse. Individual responses to CBT are as varied as the people themselves.
Approximately half of all individuals undergoing CBT treatment for social anxiety disorder report substantial reduction in social anxiety by the conclusion of therapy (Loerinc et al., 2015).
Diversity in Duration
The duration of CBT can significantly vary based on an array of factors: patient-specific challenges, therapist dynamics, and the treatment facility itself. On average, CBT for social anxiety comprises around 12 sessions.
With time, the cohort of treatment responders often expands. Approximately 10% of individuals witness the significant effects of CBT materializing post-treatment.

Maximizing CBT’s Effectiveness
If you’re on the brink of embarking on a CBT journey to combat social anxiety, there are several steps you can take to expedite its effectiveness:
- Engage candidly with your therapist, addressing your concerns openly.
- Diligently follow through with your homework assignments, embracing them as a pivotal aspect of your progress.
- Embrace exposure exercises and repeat them diligently to reinforce their impact.
- Absorb knowledge actively and proactively inquire, leveraging the therapeutic relationship.
- Cultivate the skills to become your own ‘therapist’ once treatment concludes.
E. Recommendations: CBT Workbook & Online CBT
Book Recommendation: Navigating Social Anxiety with CBT
For a comprehensive understanding of CBT for social anxiety, including numerous practical worksheets, we highly recommend the workbook “Managing Social Anxiety” (available for purchase here).
It is authored by three leading experts in social anxiety and CBT and it can be effectively used in therapy with a professional or as a standalone tool for self-improvement.
The workbook dives into the world of social anxiety encompassing situations like dating, conversations, and interviews. Condensing decades of research, the book offers actionable insights.
With user-friendly forms, relatable cases, and review questions, it merges knowledge and practical steps, paving a path towards an improved quality of life.
Recommendation: Online CBT for Social Anxiety
In recent years, the landscape of therapy has expanded to include both in-person and online options, offering individuals with social anxiety the flexibility to access treatment that suits their preferences and needs.
The ease of accessing therapy from the comfort of your own space and the elimination of geographical barriers make online therapy an attractive choice.
Research suggests that online therapy can be equally effective for treating social anxiety as in-person therapy, especially for CBT (Thew et al., 2022; Tulbure et al., 2015), and that it maintains its positive effects even after 5 years post-intervention (Hedman et al., 2011).

A compelling advantage of online therapy for individuals grappling with social anxiety is the availability of text-based sessions. This option serves as a potent antidote to intimidation, substantially reducing the barriers to stepping into therapy’s realm.
However, when considering online therapy, it’s important to ensure the platform prioritizes your privacy and security.
If you are seeking proactive steps toward alleviating social anxiety through online therapy, our foremost recommendation is “Online-Therapy“. As our esteemed partners, they stand as the top choice to guide individuals on their journey to conquer social anxiety in the digital realm.

Their platform offers a tailored experience, including 1 live session per week (video, voice, or text), unlimited messaging, an 8-section CBT program with 25 worksheets, daily worksheet replies, yoga, meditation videos, a journal, activity plan, and self-assessment tests.
You can even switch therapists easily for the right fit, all while ensuring a secure and confidential therapeutic environment.
“Online-Therapy” extends its service starting at $40 per week. Through our link provided below, you can not only explore their offerings but also enjoy a 20% discount for your inaugural month of therapy.
When registering, make sure to choose ‘individual therapy‘ and then select ‘social anxiety‘. After that, you can provide further details about your particular situation. Wishing you all the best on your journey!
F. Conclusion: Embracing Change with CBT
CBT shines as a transformative path through the labyrinth of social anxiety. By unraveling the complex cycle of thoughts and behaviors that feed this condition, CBT makes change possible.
From challenging adverse beliefs through cognitive restructuring to dismantling avoidance and safety behaviors via exposure exercises, CBT brings hope. Studies suggest that 45-55% experience substantial relief, with around 40% finding complete freedom from social anxiety post-CBT.

CBT’s swift impact is evident when exposure exercises are embraced early, yielding progress within weeks. Commitment to homework, engagement, and curiosity fuel the journey.
Furthermore, we extend an invitation to explore our complete treatment guide by clicking here. This resource not only outlines therapy choices for social anxiety, but also covers medications, lifestyle adjustments, self-help avenues, and the pivotal role of support networks.
If you’re keen on delving into the realm of medication for alleviating social anxiety, we suggest checking out our pharmacotherapy guide by clicking here.
Still have questions lingering? Then sign up for our Free 7-day Email Course; we’re here to guide you.
Beidel, D. C., Alfano, C. A., Kofler, M. J., Rao, P. A., Scharfstein, L., & Wong Sarver, N. (2014). The impact of social skills training for social anxiety disorder: a randomized controlled trial. Journal of anxiety disorders, 28(8), 908–918. https://doi.org/10.1016/j.janxdis.2014.09.016
Clark, D. M., & Wells, A. (1995). A cognitive model of social phobia. In R. G. Heimberg, M. R. Liebowitz, D. A. Hope, & F. R. Schneier (Eds.), Social phobia: Diagnosis, assessment, and treatment (pp. 69–93). The Guilford Press.
Hedman, E., Furmark, T., Carlbring, P., Ljótsson, B., Rück, C., Lindefors, N., & Andersson, G. (2011). A 5-Year follow-up of internet-based cognitive behavior therapy for social anxiety disorder. Journal of medical Internet research, 13(2), e39. https://doi.org/10.2196/jmir.1776
Heimberg, R. C., Brozovich, F. A., & Rapee, R. M. (2014). A cognitive-behavioral model of social anxiety disorder. In S. G. Hofmann & P. M. DiBartolo (Eds.), Social anxiety: Clinical, developmental, and social perspectives (pp. 705–728). Elsevier Academic Press. https://doi.org/10.1016/B978-0-12-394427-6.00024-8
Loerinc, A. G., Meuret, A. E., Twohig, M. P., Rosenfield, D., Bluett, E. J., & Craske, M. G. (2015). Response rates for CBT for anxiety disorders: Need for standardized criteria. Clinical psychology review, 42, 72–82. https://doi.org/10.1016/j.cpr.2015.08.004
Springer, K. S., Levy, H. C., & Tolin, D. F. (2018). Remission in CBT for adult anxiety disorders: A meta-analysis. Clinical psychology review, 61, 1–8. https://doi.org/10.1016/j.cpr.2018.03.002
Thew, G. R., Kwok, A. P. L., Lissillour Chan, M. H., Powell, C. L. Y. M., Wild, J., Leung, P. W. L., & Clark, D. M. (2022). Internet-delivered cognitive therapy for social anxiety disorder in Hong Kong: A randomized controlled trial. Internet interventions, 28, 100539. https://doi.org/10.1016/j.invent.2022.100539
Tulbure, B. T., Szentagotai, A., David, O., Ștefan, S., Månsson, K. N., David, D., & Andersson, G. (2015). Internet-delivered cognitive-behavioral therapy for social anxiety disorder in Romania: a randomized controlled trial. PloS one, 10(5), e0123997. https://doi.org/10.1371/journal.pone.0123997

About the Author: Martin Stork
Martin is a professional psychologist with a background in physical therapy. He has organized and led various support groups for people with social anxiety in Washington, DC and Buenos Aires, Argentina. He is the founder of Conquer Social Anxiety Ltd, where he operates as a writer, therapist and director. You can click here to find out more about Martin.